I was lucky to be able to enter the OT to see an open heart surgery for CABG.
This patient had Percutaneous Coronary Intervention (stenting) done before but then it's not working anymore and that artery that received PCI had narrowed down. So the surgeons have to replace the narrowed artery and create a collateral branch for it for collateral perfusion.
Patient came in at 8am and got prep for surgery.
First, neck line was set up. They had trouble setting it on the left side so they changed it to the right. While at it, the surgeon marked the surface marking for harvesting the great saphenous vein at the right inner thigh.
Second, urinary catherization.
Third, skin preparation. Basically, sterilization. I guess it's to avoid any pathogens to enter the body through the incisions they were gonna make later.
And of coz, syringes with medications, surgery equipments which I couldn't name and monitoring equipments to monitor the patient's time to time status.
At last, they started the surgery at 9.40am.
There were 4 surgeons doing the surgery. 2 harvesting the great saphenous vein, 1 (main surgeon) harvesting the internal mammary artery and 2 (main surgeon and another surgeon) doing the CABG.
The main surgeon made an incision on the midline of the chest- sternotomy. This will then expose the sternum. The surgeon then used an equipment which worked like a saw to cut open the sternum into half to reach the thoracic cavity. The saw the left lung from the place where i was seeing.
Great saphenous vein harvesting:
The surgeons made 2 separate incisions on the right inner thigh. One is above the knee, and the other one is about 3 fingers above the first incision. When they incised the thigh and initially exposed the great saphenous vein, it was a bit BLUISH! :D and then it turned slightly red. The great saphenous vein is quite big. It's like a white colour wire when they took it out. Diameter is around 3mm? The length they harvested is about 10cm i think. I am not very sure. They ligated the smaller veins that previously drained into it and removed it from the inner thigh.
Internal mammary artery harvesting:
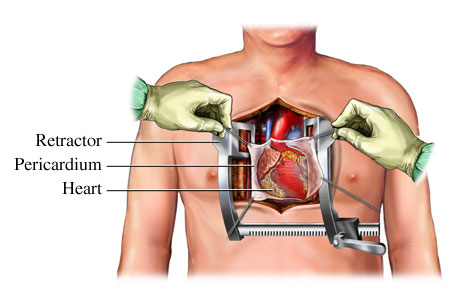
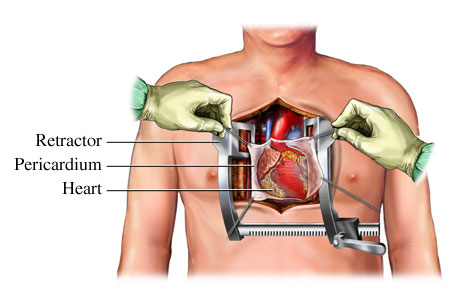
MAN! This is so cool! This is like the happiest day of my life. WHY? I got to see the heart and lungs IN SITU! with the sternum cut open to expose them.The chest was opened up using a retractor. The was chest wide open and u can actually see all the layers. and there, when the surgeon was harvesting the left internal mammary vein, the innermost layer of the chest just above the lungs. I COULD SEE THE LEFT LUNG EXPAND. It's such a historical moment-for me. I could clearly see that the left lung has 2 lobes. However, I didn't get to see the lingula. URGH!
After the harvesting, the surgeons who were responsible for taking out the great saphenous vein put the vein in the kidney dish and sew up the incisions. While the main surgeon and another surgeon worked their way through the pericardium to reach the heart.
They opened the pericardial sac and push it aside, exposing the right atrium (I could see the right auricle too), the right ventricle, the aorta and the pulmonary artery. :D The heart is enveloped by a layer of thick fat tissue. The surgeons then lifted the heart and also started the bypass grafting. Amazing! The surgeon used this super fine thread to stitch the super fine vein when the end of it was a little bit torn. SALUTE! They have this special glasses so I guess that helped them to magnify the fine broken part of the vein when they were stitching. After that the remaining main process was to anastomose the internal mammary artery and the great saphenous vein on the surface of the heart.
At the end of the procedure, which was almost 4 hours in the OT, CABG was finally done and the surgeon used this thick sternal wire to stitch the sternum back together and close the incision.
Open heart surgery is always an impressive surgery to me.
What I learnt:
1. In the OT, never turn ur back against the sterile equipment.
2. Stand one foot away from the sterile equipment.
3. The low temperature, around 16 degree celcius is compulsory to reduce the risk of infectious pathogens being active and infect the opened chest.
4. CABG- they use great saphenous vein and internal mammary artery.